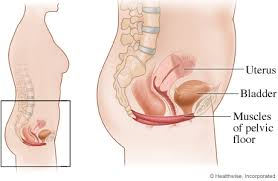
Is pelvic floor weakness linked to the vaginal microbiome?
I couldn’t help being magnetically pulled into the reported findings of this study: that postpartum vaginal microbiome imbalance was associated with weaker pelvic floor muscles. What?! A study that finds a connection between two of my apparently disparate clinical interests?! I just had to know more, so I dug into the study…
Is pelvic floor weakness – or urinary incontinence – connected to imbalance in the vaginal microbiome?
This study evaluated the vaginal microbiome in 6-8/52 postpartum women, taking 183 vaginal swabs. Unusually, the women were prospectively divided into 2 groups: Stronger Pelvic Floor and Weaker Pelvic Floor (it seems they defined Stronger Pelvic Floor as a peak pressure >35cm H20 on voluntary pelvic floor contraction via a pressure probe).
While we need to gloss over in-depth detail, the finding about vaginal Lactobacillus is interesting.
(Warning: boring bit only for evidence-minded clinicians.)
While the use of 16SrRNA technology to characterize the vaginal microbiome wasn’t ideal, because of its inability to accurately identify to species level, we can accept it in this case. This is because genus-level distinctions (i.e. dominance by Lactobacilli or not) are still meaningful in the vaginal microbiome, even if not as informative as the species of Lactobacilli. It is also important that any microbiome research use a statistical test for multiple comparisons. While this wasn’t stated anywhere in the paper, when I hunted through the Supplementary Data spreadsheets they stated a q-value – which usually reflects an FDR correction, so I think we can safely assume it was done. (This is important, because if it isn’t done, then any significant p-values we see may indicate spurious associations.)
(OK, back to the substance.)
So what were the associations they found?
The incidence of urinary incontinence was significantly higher in the Weaker Pelvic Floor group. (No great surprise).
The real surprise comes in the finding of the difference in vaginal Lactobacillus between groups.
Differences in abundance in Lactobacillus between groups was implied but hard to find in the text of the paper. By hunting through the Supplementary tables, I could see that the relative abundance of Lactobacillus genus in the Strong Pelvic Floor group was around 24%, and almost four times higher than that of the Weak Pelvic Floor group. Reassuringly, this was significant at a q-value of <0.009, so is likely to reflect a real difference between the groups.
Vaginal lactobacillus levels were almost four times higher in the “Strong Pelvic Floor” group.
(By the way, 7% and 24% may sound very low for Lactobacillus levels in the vagina, but remember that these women are 6-8 weeks postpartum and likely have very low estrogen levels. Unfortunately, the investigators don’t tell us breastfeeding rates – and in fact this is very important, because if lower in the Strong Pelvic Floor group, this could be an explanation for higher Lactobacillus levels).
However, when they looked at those with urinary incontinence vs those without urinary incontinence, there was no statistically significant difference in lactobacillus levels.
Strengths of the study include…
- Interest value! What a novel topic. So refreshing to see a new link being explored between two very important aspects of pelvic health!
- The appropriate application of a multiple comparisons correction, as shown by their (albeit subtle) reporting of p-values
- The fact they controlled for potential confounders of the difference in vaginal microbiome, including antibiotic use, BMI, presence of persisting lochia, reproductive tract infection, sexual intercourse and vaginal irrigation
So this study was interesting, statistically advantageous, and reasonably well-controlled.
What I wish they had done…
- Recorded and compared breastfeeding status between groups
- Speculated a bit more logically – with accurate rather than spurious citations* – about a potential cause for the difference they found.
- Use the more accurate shotgun metagenomics technology for a more detailed, reliable picture of the vaginal microbiome
I love seeing more vaginal microbiome research, so I don’t want to get nitpicky. Seems like we can watch this space for more novel associations being explored!